On December 30, 2019, Dr. Li Wenliang, an ophthalmologist at Wuhan Central Hospital in the Hubei province of China, messaged his fellow physicians, alerting them to the appearance of what he thought as SARS. Thirty-nine days later, after becoming infected with the very virus he tried to warn his colleagues about, he was dead at thirty-three. By that time, the disease we now know as COVID-19 had already spread to dozens of countries.
Before the SARS outbreak in 2002, only two coronaviruses were known to cause disease in humans, but neither caused much more than the common cold. The SARS coronavirus, however, went on to kill about one in ten people it infected. A decade later, in 2012, MERS, another deadly coronavirus, emerged. Like SARS, MERS spread to infect thousands of people across dozens of countries, but that time, one in three died. Today, we’re fighting to protect ourselves from—and to defeat—the COVID-19 coronavirus.
Where are these emerging infectious diseases emerging from?
All human viral infections are believed to originate in animals.
To understand COVID-19 and other deadly viral outbreaks, we have to understand their history and evolution if we’ll ever have a chance at preventing future pandemics. We also have to look back and take lessons from the past. How did we successfully beat back SARS? Why is it more difficult with COVID-19? What do we have to do to slow the pandemic today before we even have a hope at a vaccine?
I covered all of that in my recent four-hour webinar—from origin stories of past killer pandemics to what we should be doing today to stay safe—and then dove into the clinical side of COVID-19 and discussed what the disease looks like and the best way to treat it. If you missed the webinar, the following is an overview of what I covered.
FROM THE BEGINNING
The Emergence of MERS
- Most human coronaviruses appear to have arisen originally in bats, thought to be the primordial hosts, but jumping the species barrier to infect people appears to require intermediate hosts.
- In the case of MERS, the intermediate hosts were found to be camels.
- Although we domesticated camels three thousand years ago and MERS had long been circulating in them for decades without crossing the species barrier into humans, more recent intensification of camel production—from foraging outdoors to, today, primarily being confined indoors at high stocking densities—is thought to be what helped drive the spillover of MERS from camels to people.
- The first human cases of MERS were reported in 2011, the year after open grazing was banned in Qatar, the Middle Eastern country with the highest camel density.
The Emergence of SARS
- The first new global disease outbreak of the 21st century was SARS, even before MERS.
- In the case of SARS, the intermediate hosts were found to be civet cats.
- SARS-CoV causes the SARS coronavirus, and SARS-CoV-2 causes the COVID-19 coronavirus.
- Many of the first cases of SARS were found in the same type of place most of the first cases of our current COVID-19 pandemic have been found: live animal “wet” markets in China.
- At wet markets, crowded cages of animals, including exotic animals, are contaminated with the feces, urine, and blood of different species mixed together, and animals may be slaughtered. These conditions lead to a perfect storm for zoonotic (animal-to-human) disease transmission.
- The virus uses the spikes on its corona like a key in a lock to access host receptors. Just as a new lock needs a new key, in order to switch from infecting one species to another, the genes coding the spikes must mutate to fit into the new host’s receptors.
- Both viruses that cause SARS and COVID-19, SARS-CoV and SARS-CoV-2, respectively, attach to an enzyme coating the cells of our lungs. By the time bat coronaviruses made it into civets, the virus’s docking spikes were just two mutations away from locking in the configuration to bind to human receptors—and then the human-to-human SARS epidemic was born.
The Emergence of COVID-19
- Ground zero for the COVID-19 pandemic was the Hua’nan Market in Wuhan, China, named in Dr. Li’s “7 SARS cases confirmed” message. It wasn’t a SARS-coronavirus, though. It was a virus to be named SARS coronavirus 2 (SARS-CoV-2), the cause of coronavirus disease 2019, or COVID-19.
- The new COVID-19 coronavirus is about 80 percent identical to the original SARS virus, but it’s more than 95 percent identical to a coronavirus found in a bat in 2013.
- The current theory: COVID-19 originated in bats before jumping to humans after passing through an intermediate host, thought to be the pangolin, the most trafficked mammal in the world.
- Coronaviruses found in two different groups of diseased pangolins being smuggled into China were found to be about 90 percent identical with the COVID-19 virus. As well, the pangolin coronavirus spike protein’s critical receptor binding region is virtually identical to the human strain.
Coronaviruses Infect Pigs Right Off the Bat
- COVID-19 is the fourth coronavirus to jump from bats to cause large deadly outbreaks in the 21st century. First was SARS in 2002, MERS in 2012, and then SADS—Swine Acute Diarrhea Syndrome—in 2016, which devastated commercial pig farms in the same part in China where SARS had broken out. SADS was traced to a coronavirus discovered in a nearby bat cave.
- Other emerging and re-emerging coronavirus diseases include Porcine Epidemic Diarrhea and Porcine Deltacoronavirus among pigs, and Infectious Bronchitis Virus in chickens. Increasingly, coronaviruses are emerging and circulating among farm animal populations, and the more novel coronaviruses mix in greater numbers of animals, the greater the likelihood that strains with the potential to spark a pandemic may emerge.
COVID-19 May Not Have Been the First Coronavirus Pandemic
- The second most common cause of the common cold are coronaviruses.
- To date, four human cold coronaviruses have been discovered, which means seven coronaviruses in all can cause human disease as far as we know. We believe we got SARS from civets, MERS from camels, and COVID-19 perhaps from pangolins.
- Though we still don’t know where two of the four mild coronaviruses originated, one—human coronavirus 229E—has been traced back to camels and the other—OC43—traced back to cattle or pigs.
- Molecular clock analyses dating human coronavirus OC43’s emergence suggest that the bovine coronavirus now causing “shipping fever” disease in cattle, jumped to humans around 1890. Indeed, that same year, 1890, there was a pandemic, presumed to be influenza.
- Because of the timing of the emergence of human coronavirus OC43, some conjecture it actually may have been a COVID-19-like interspecies transmission of a coronavirus. This is supported by the fact that cattle herds the world over were being devastated by a deadly respiratory disease, resulting in massive culling operations between 1870 and 1890.
PUMPING THE BRAKES
Slowing an Outbreak
- There were more COVID-19 cases in the first month of reporting than SARS ever caused. Why? The primary reason revolves more around when it is contagious than how contagious it is.
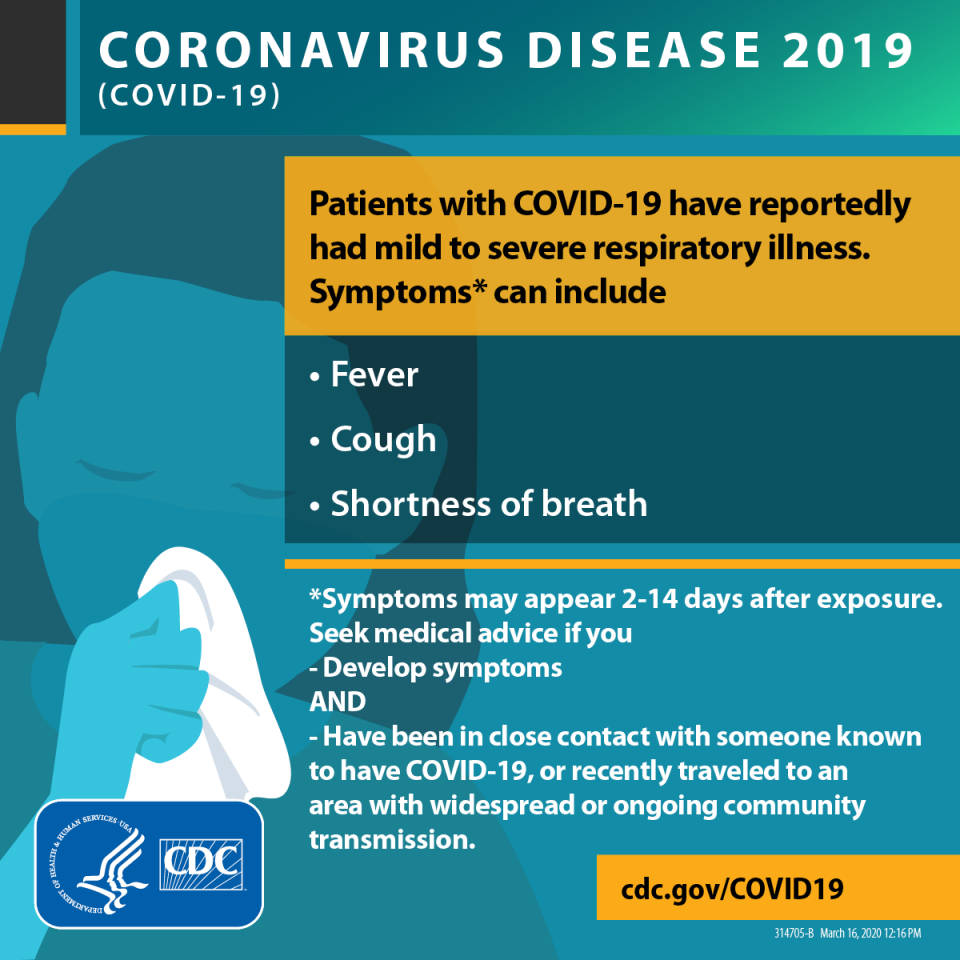
- Microbes most likely to cause pandemics have three characteristics: (1) novelty, therefore, without pre-existing immunity; (2) respiratory spread; and (3) transmission before the onset of symptoms.
- SARS, despite spreading to twenty-nine countries and regions, was not considered a pandemic. And, we were able to stop it within only a few months, after approximately 8,000 cases and 800 deaths. Why? SARS was spread via respiratory droplets but lacked significant spread before symptoms arise.
- SARS’s average incubation period—from first becoming infected to first coming down with symptoms—was around five days, but viral loads took another six to eleven days to ramp up. So, SARS patients weren’t very infectious in the first five or so days of the illness. In that way, transmission from person to person could be stopped if patients were isolated within the first few days after symptoms arose.
- One hundred percent of SARS patients developed a fever, as did 98 percent of MERS patients. However, as many as 36 percent—more than one in three—of COVID-19 patients do not present with fever at the onset of symptoms and, more seriously, may be infectious while completely symptom-free during the incubation period.
- People can potentially spread COVID-19 before even knowing they have it, even while they’re feeling completely fine, which is why isolation may slow the spread of disease without knowing who is infectious.
Slowing a Pandemic
- China enacted “wartime control measures” and initiated the most expansive containment effort in history, affecting about three quarters of a billion people, confining them to their homes.
- The seemingly impossible was achieved: the containment of a widely circulating respiratory infection. Ground zero of COVID-19, Hubei Province, reported its first day of no new local cases within two months.
- That same day, the world confirmed its 200,000th
- Countries able to rapidly control the disease quickly relied on testing and tracing—mass testing to identify all cases and tracing every patient’s every possible contact—to block as many paths of transmission as possible through isolation and quarantine.
- Rapid response varied wildly. By the middle of March, South Korea had tested more than a quarter million people, more than five thousand out of every million citizens, compared to fewer than a hundred per million in the United States.
- When the window on containment closes, as it did in the United States, the strategy pivots to suppression and mitigation.
- Closing nonessential businesses, cancelling gatherings, and encouraging people to stay at home and shelter in place all attempt to break every possible link in the chain of viral transmission—to “flatten the curve,” that is, to flatten the epidemic curve to slow the spread of disease to more evenly distribute the cases over time.
- Until there is wide availability of an effective vaccine, thought unlikely until 2021 at the earliest, population lockdowns can help slow the spread by removing susceptible hosts from the virus’s reach. Once such stay-at-home measures are relaxed, though, the disease could attack again as it did in the 1918 pandemic when some U.S. cities suffered a second peak in mortality after social-distancing measures were lifted.
- Triage protocols have been published, establishing a hierarchy of care in anticipation of too few resources, such as hospital beds and ventilators, and too many patients. Wrote a preeminent group of medical ethics experts in the New England Journal of Medicine, “[W]e believe that removing a patient from a ventilator or an ICU bed to provide it to others in need is also justifiable and that patients should be made aware of this possibility at admission,” adding, “the decision to withdraw a scarce resource to save others is not an act of killing and does not require the patient’s consent.”
TREATING AND AVOIDING COVID-19
The Clinical Course of COVID-19
- COVID-19 is thought to have an average incubation period of about five days, which means we are infected and possibly infectious for almost a week before we may even know we have the disease.
- Not all infected people show symptoms, but of those who do, about 98 percent start exhibiting them by day twelve, which explains why quarantine after a potential exposure are for two weeks.
- After infection, the virus may shed for more than a month (with an average of twenty days), but it is unclear how contagious survivors are during that period.
- The most common symptoms are fever (90 percent of patients) and cough (70 percent). About four in ten experience fatigue, three in ten cough up phlegm, two in ten have muscle aches, and one in ten may suffer gastrointestinal symptoms, such as nausea or diarrhea, or common cold-type symptoms, like runny nose, sore throat, or headache.
- Difficulty breathing has been the only symptom found predictive of a more severe course of COVID-19 and has resulted in more than six times the odds of eventually being admitted into the ICU.
- COVID-19’s severity varies widely based on pre-existing conditions: People with high blood pressure are twice as likely to suffer a severe course and three times as likely with cardiovascular disease, and those with either condition are about four times as likely to end up in the ICU. Those with chronic obstructive pulmonary diseases (COPD) like emphysema appear to be at the highest risk (six times the odds of a severe course) and nearly eighteen times the odds of ICU admission.
- As with SARS and MERS, those with diabetes appear to be at higher risk.
- Excess body fat also seems to be a risk factor. Those with a body mass index (BMI) of 28 or more appear to have nearly six times the odds of suffering a severe COVID-19 course. (The average BMI in the United States exceeds 29)
- Even without taking weight into account, most adult Americans over fifty suffer from a “co-morbidity” that may put them at risk. It’s important to note that the major comorbid conditions for COVID-19 severity and death—obesity, heart disease, hypertension, type 2 diabetes—may all be controlled or even reversed with a healthy enough plant-based diet.
- Although newborns through seniors in their nineties have been infected, most COVID-19 patients are between thirty and seventy-nine, but the severity of the disease disproportionately affects older patients. Compared with people aged nineteen to sixty-four, in the United States, those sixty-five and older without underlying conditions or other risk factors appear to be hospitalized or end up in the ICU at approximately three times the rate.
- The best data come from South Korea: Of confirmed cases, about 1 in 1,000 died in their thirties and forties, 1 in 150 of those in their fifties, 1 in 50 in their sixties, 1 in 15 in their seventies, and 1 in 5 in their eighties. U.S. data are less reliable due to the relative lack of testing, these age-related death risks are similar based on the first few thousands of American cases that were reported.
- On autopsy, the lung’s respiratory surface appears obliterated by scar tissue. Pulmonary fibrosis (lung scarring) is expected to be a long-term complication among survivors of serious COVID-19 infection.
- Death from COVID-19 is the result of progressive “consolidation” of the lung—your lungs start filling up with something other than air. In COVID-19 pneumonia, postmortems show you drown in lungs “filled with clear liquid jelly.”
How to Treat COVID-19
- Presently, there is no specific proven therapy for COVID-19.
- Although there are more than 400 clinical treatment trials underway, we should not expect an effective antiviral drug or vaccine anytime soon.
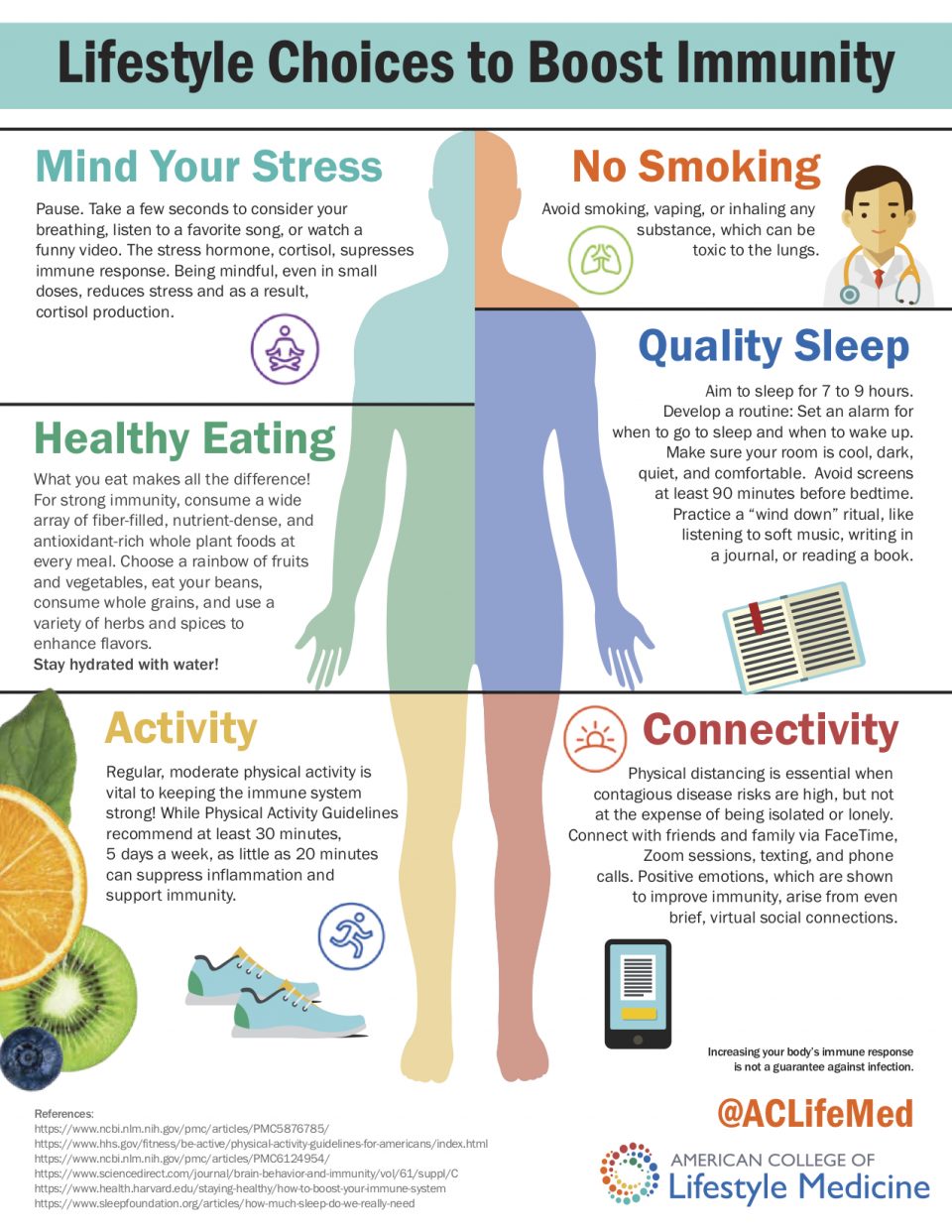
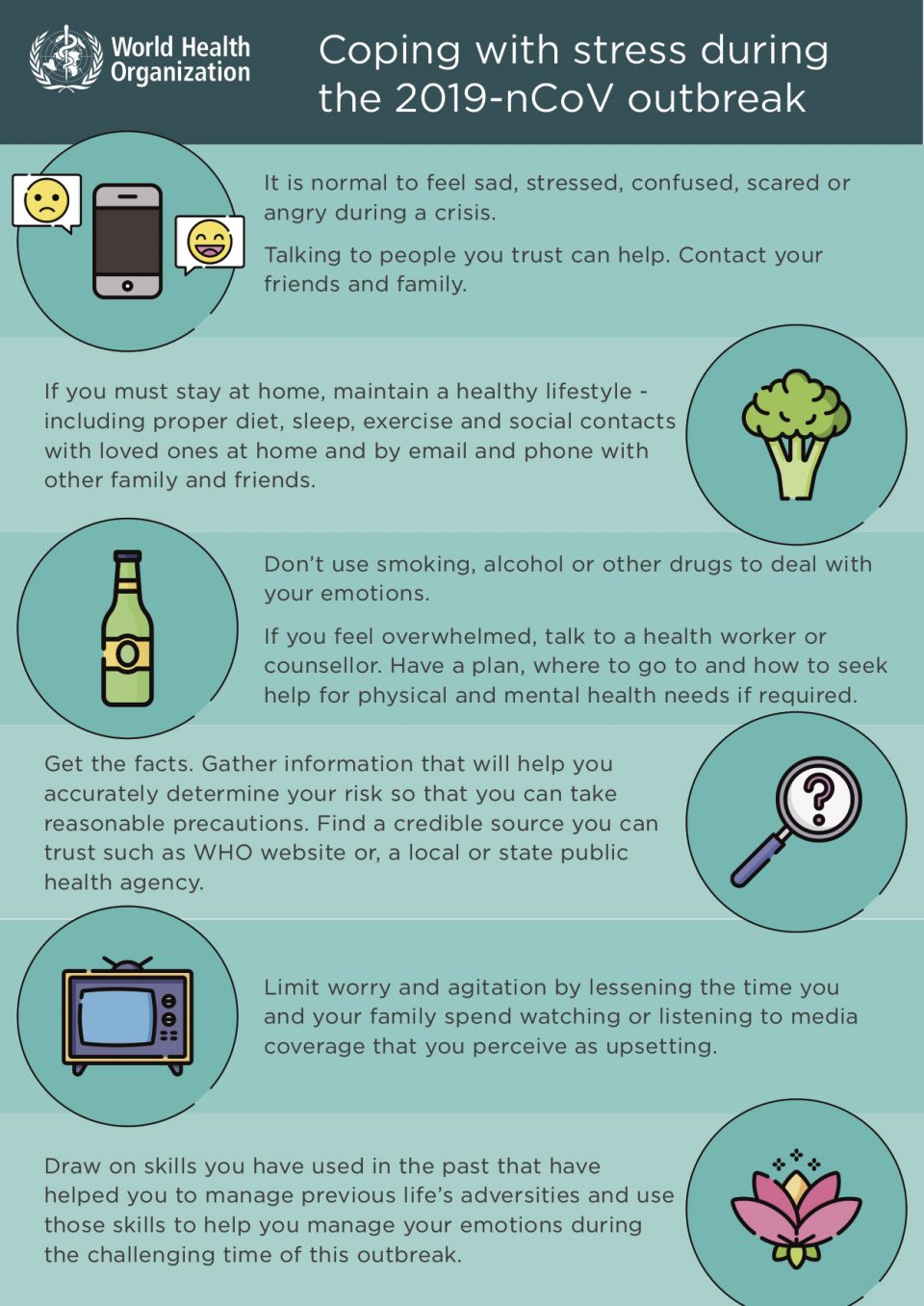
- I support commonsense advice to stay healthy during the crisis, as recommended by trusted authorities such as the American College of Lifestyle Medicine and the World Health Organization, including getting sufficient sleep (seven to nine hours), reducing stress, keeping active, staying connected (remotely) to friends and family, and eating healthfully (a diet centered around whole plant foods).
- Given our near-total ignorance of the immunological aspects of COVID-19, I will not jump on the snake-oily spamwagon to promote foods to boost immunity. We just don’t know if enhancing specific arms of the immune system could make things even worse.
- There is an assumption that seniors are more susceptible to serious COVID-19 courses due to their waning, aging immune systems, but that may not be correct. Similarly, though young children, with their relatively immature immune systems, typically suffer disproportionally from infections such as the flu, that doesn’t appear to be with the case with COVID-19 (or SARS or MERS). Likewise, immunosuppressed patients may not be at greater risk of severe complications from COVID-19, although they normally are from respiratory viruses.
- Our own immune response may be the primary driver of damage to the lungs during coronavirus infection—somewhat akin to an autoimmune reaction where the body over-reacts and the lungs get caught in the crossfire as the coronavirus is attacked.
How to Avoid COVID-19
- Although cancelling gatherings, meetings, and events may slow COVID-19’s spread by as much as 35 percent, according to preliminary evidence from Japan, that has not been enough to contain the outbreak.
- Our best course of action is to shelter-in-place—stay home to reduce contact with those outside our households as much as possible—and to do so now.
- By the time a community has its first death from the disease, it’s likely that hundreds or even thousands of cases are present.
- If you must leave your home to provide essential services such as direct care or food delivery, maintain a safe distance from others and sanitize your hands every time you touch a public surface. It’s critical not to touch your mucous membranes—your eyes and the inside of your nose or mouth—with unsanitized hands.
- The virus can’t pass through your skin. It can only replicate in live cells, and our skin’s outer layer is covered by protective dead skin cells. To get into your lungs, the virus has to find its way to your mucous membranes, the moist lining of your eyes, nostrils, or mouth.
- To the best of our current understanding, the COVID-19 coronavirus is thought to be transmitted from person to person via respiratory droplets coughed out by the infected into the air and then landing in the eyes, nose, or mouth of another. You can also infect yourself by touching your eyes, nose, or mouth with hands contaminated by a virus-laden object or surface—for instance, by picking your nose or rubbing your eyes after shaking someone’s hand or touching a public surface like a door knob or an elevator button.
- The levels of virus in the snot of COVID-19 patients can reach almost a million per drop.
- The COVID-19 coronavirus has been detected in stool samples, suggesting another way toilets may potentially transmit infection, beyond just touching the flush handle. Modern flush toilets aerosolize up to 145,000 droplets of toilet water into the air, which can float around for at least thirty minutes, so be sure to close the lid before you flush and then, of course, thoroughly wash your hands.
- Coronaviruses are “enveloped” viruses. As they emerge from our infected cells, they cover themselves in the outer layer of our cells. Although that oily coating makes it harder for our immune system to detect them because they look like us, it also makes them susceptible to disinfection and environmental inactivation.
- The COVID-19 virus appears to survive for less than three hours on printing paper but may last for one day on cloth. On the outer layer of surgical masks, though, it can survive for a week. COVID-19 virus’s half-life is about six hours on steel or plastic, so, although about 99 percent is gone by forty-eight hours, it may be up to 96 hours for all infectivity to be extinguished.
How to Inactivate COVID-19
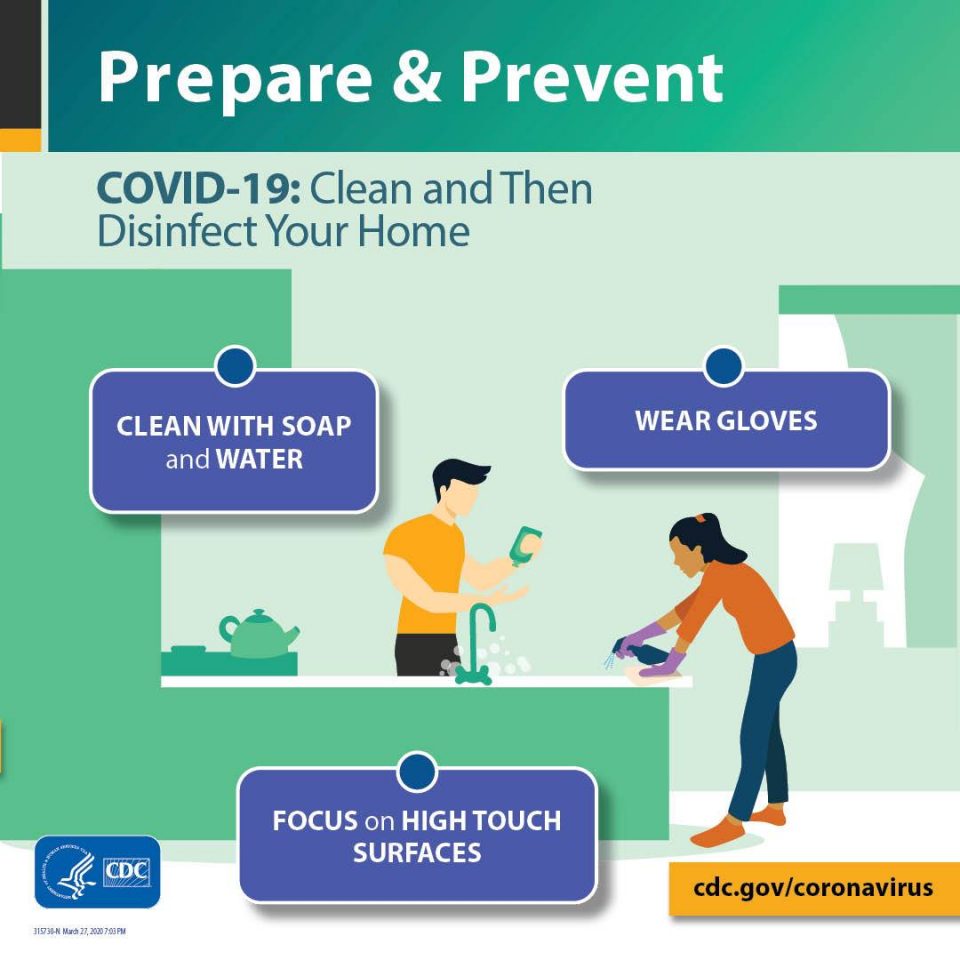
- Hands can be disinfected by properly washing your hands with soap and water. The CDC recommends washing them for at least twenty seconds. Researchers found the fingertips, thumbs, and backs of hands are the most frequently missed areas when washing, so be sure to wash thoroughly.
- There is no need to use hot water when washing your hands.
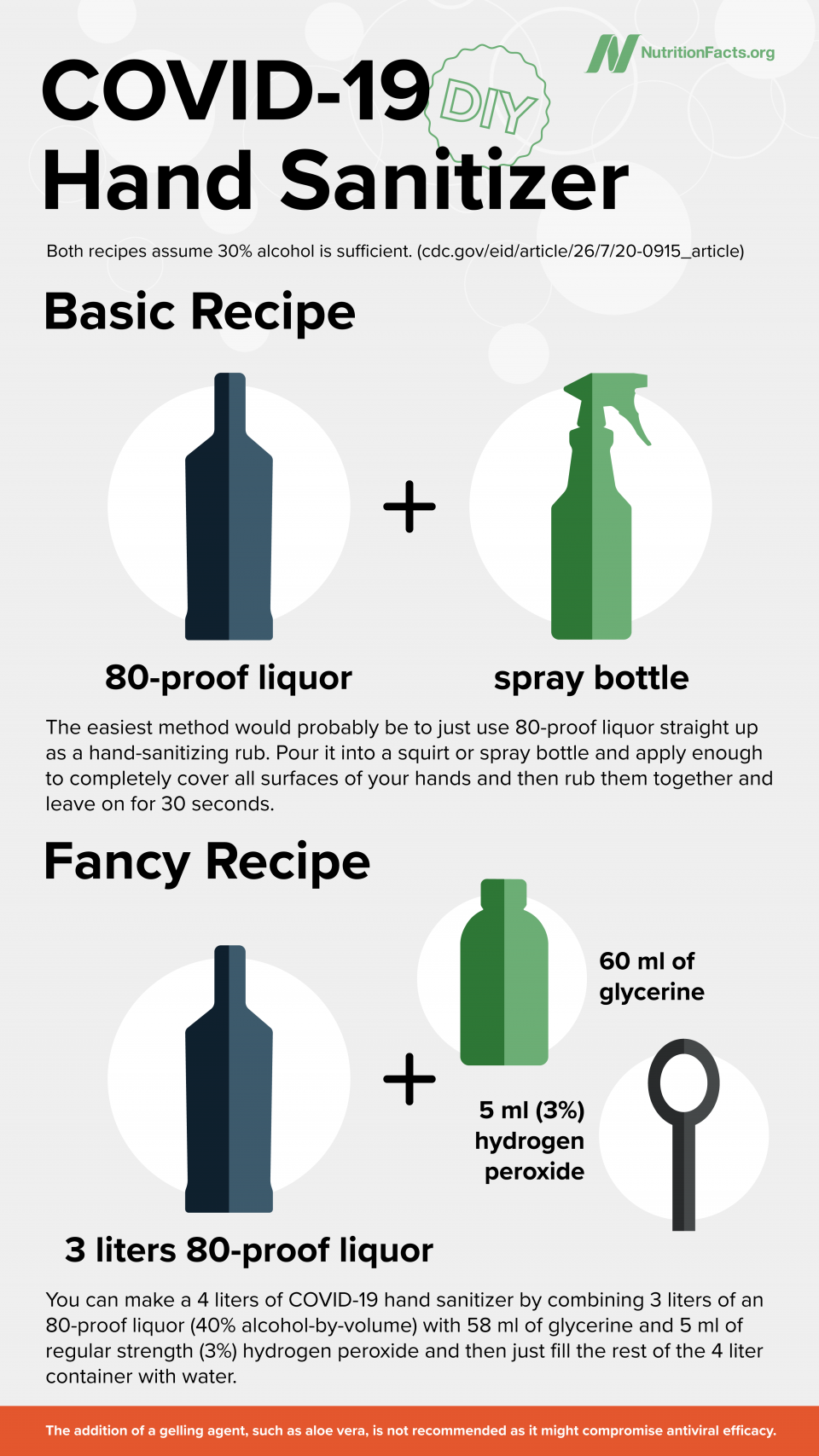
- Researchers found that the COVID-19 virus could be inactivated within thirty seconds by 30% alcohol (ethyl or isopropyl). Most vodka, rum, brandy, gin, and whisky exceed 30% alcohol by volume. Note that 30% alcohol isn’t enough to kill many other pathogens, so I still recommend sanitizers with 60% to 80% alcohol. (One rub to rule them all!) But, if you can’t find them, it’s nice to know you can make your own.
DIY Hand Sanitizer
Basic Recipe: The easiest method would probably be to just use 80-proof liquor straight up as a hand-sanitizing rub. Pour it into a squirt or spray bottle and apply enough to completely cover all surfaces of your hands and then rub them together and leave on for 30 seconds. The addition of a gelling agent such as aloe vera is not recommended as it might compromise antiviral efficacy.
Fancy Recipe: Assuming you have all of the ingredients, you can make a gallon of COVID-19 hand sanitizer by combining 12 cups of an 80-proof liquor (40% alcohol-by-volume) with ¼ cup of glycerine (also spelled glycerin or called glycerol) and a teaspoon of regular strength (3%) hydrogen peroxide and then just fill the rest of the gallon container with water. To make just a quart, simply quarter the recipe: 3 cups liquor, 1 tablespoon glycerine, ¼ teaspoon hydrogen peroxide, and water. Again, don’t add anything else.
- Bleach is recommended for disinfection of inanimate surfaces—1 part household bleach diluted in 49 parts water, so about 1 teaspoon bleach per cup of water.
- This 1:50 recommendation is for standard bleach (5% sodium hypochlorite). If you have 2.5% hypochlorite bleach, use two teaspoons per cup, and if you have 10% hypochlorite bleach, you only need a half teaspoon per cup.
- Prepare the bleach solution fresh and leave it on the surface you’re disinfecting for at least ten minutes. Surfaces visibly contaminated with bodily secretions like snot, blood, or poop may require a stronger bleach solution (1 part standard bleach to 9 parts water, left for ten minutes).
- NEVER mix bleach with any other cleanser as it reacts with ammonia (found in many glass cleaners) to create hazardous gases and reacts with acids (like vinegar, or some toilet bowl, drain, and automatic dishwashing detergents) to create chlorine gas, which is also toxic.
(click to enlarge: imperial & metric)
What If You Come Down with COVID-19?
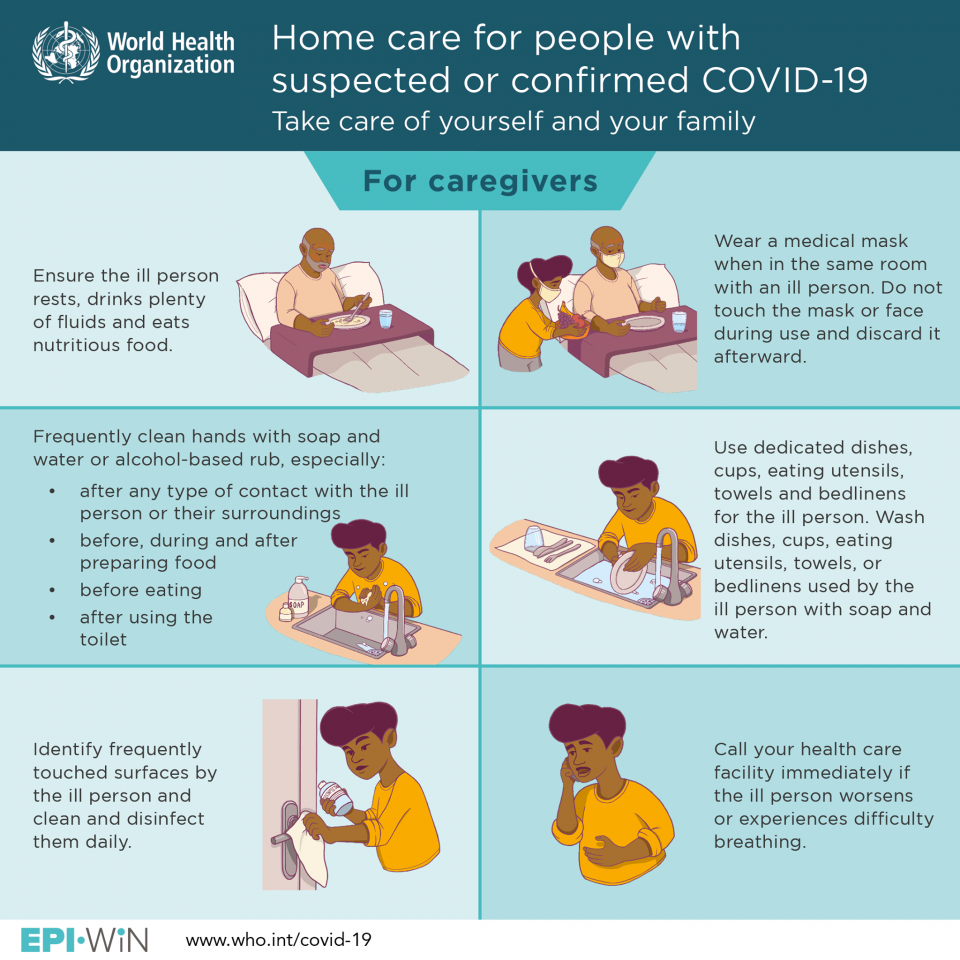
- The best option is to try to recover at home, isolated as much as possible from others in your household. Preferably, you should avoid contact with both people and pets, and be cordoned off in a “sick room” with a separate bathroom if possible.
- Most people who get infected with the COVID-19 virus recover without medical intervention. If you do come down with it, protect those around you, rest, hydrate, and monitor your symptoms. If you experience difficulty breathing or persistent pain or pressure in the chest, seek medical attention—but, first call your doctor or emergency room before heading in, since they may have special instructions for suspect cases in your area.
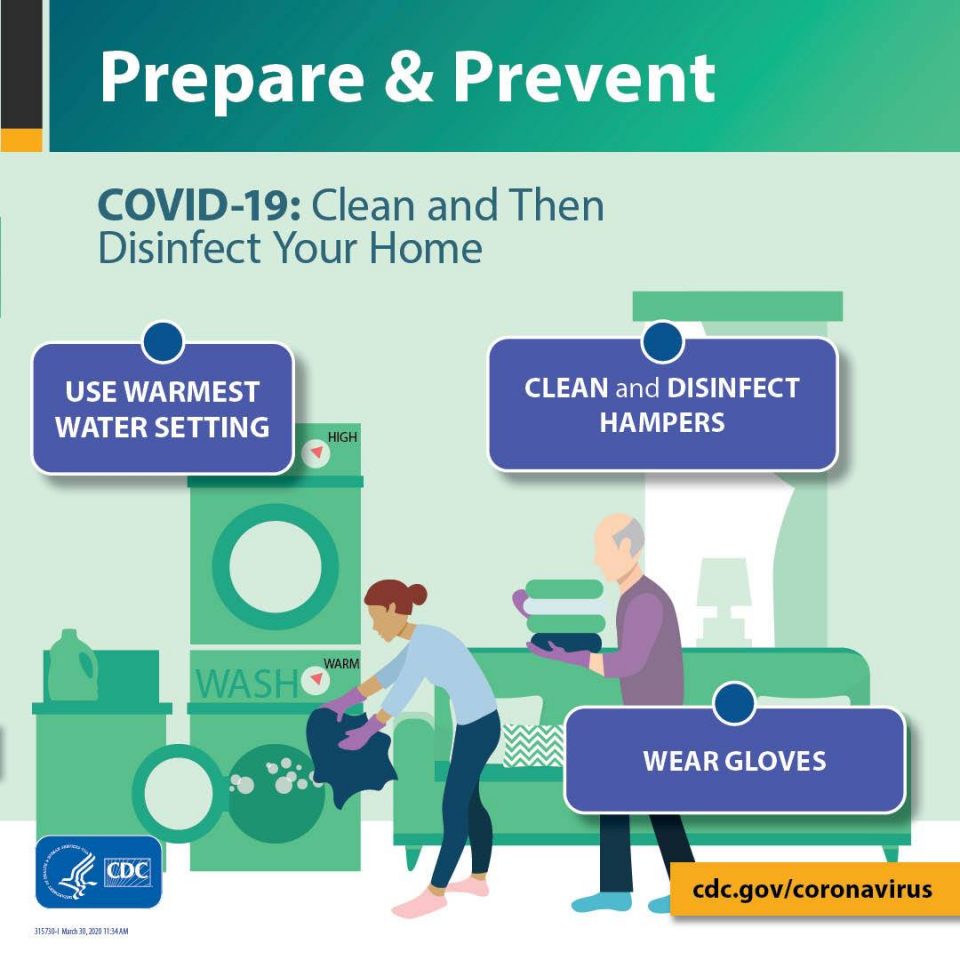
- Practice good hygiene and social-distancing etiquette: Wash your hands often. Cough or sneeze into a tissue, covering your nose and mouth, then throw the used tissue into a lined bin and immediately sanitize your hands. Don’t share eating utensils, towels, bedding, or other personal household items. Routinely disinfect all high-touch objects (e.g., doorknobs and toilet surfaces) in your sick room and bathroom yourself, but have someone else disinfect the rest of the house. Be sure to wear gloves while cleaning and disinfecting, and open windows if possible and wear a surgical mask.
- If you’re sick but must share a room with someone else, wear a face mask. That’s what they were originally designed for: source control, rather than self-protection.
(click to enlarge)
- It’s important to understand that respiratory droplets are not just gobs of mucus. When you’re outside on a cold day and your breath fogs, those are respiratory droplets. That vapor plume you’re exhaling is made up of tiny water droplets straight from your lungs. On a warm day, you breathe out that same cloud—you just can’t see it.
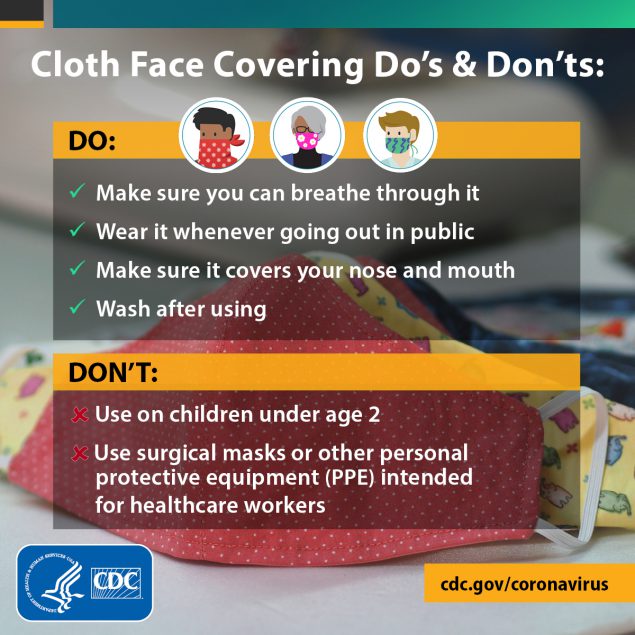
- Should everyone cover their face in public since infected individuals are exhaling virus before they even know they have it? The CDC recommends “wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain” such as grocery stores or pharmacies. The U.S. Surgeon General is featured in a video demonstrating how to improvise masks out of a bandana and rubber bands, and the CDC has easy no-sew instructions at bit.ly/CDCDIY.
(click to enlarge)
- Cloth coverings, which should be washed regularly, are no substitute for masks, but may be better than nothing. Scarves, pillowcases, and 100 percent cotton t-shirts are probably the most suitable household materials for making homemade masks, blocking various bacteria and viruses about 60 percent as well as surgical masks.
- What about N95 masks? Also known as N95 respirators, these are cup-like masks that fit tighter to the face and, unlike surgical masks, are intended to protect the wearer. The CDC and its European counterpart recommend N95 masks for healthcare workers during routine care of patients, while the World Health Organization suggests surgical masks are sufficient.
- Until we know more about how the COVID-19 virus is transmitted, it seems prudent for those in close contact with coughing patients use eye protection (at least a face shield) and N95 respirators.
- According to the CDC, once your symptoms start improving, you’ve been fever-free for three full days off of fever-reducing medicines, and it’s been at least one week since your symptoms first appeared, only then can you start relaxing your home isolation. The World Health Organization is more conservative, though, and recommends self-quarantine for a full fourteen days for anyone with symptoms or living with anyone with symptoms.
- A note on pets: Dogs have been found infected with the COVID-19 coronavirus in rare cases, but it replicates poorly in dogs and doesn’t seem to make them sick, and they don’t appear to pass the virus along to others. In cats, however, the virus has been shown to reproduce And, cats have been able to experimentally transmit the virus to other cats even though they may not themselves become sick. In the United States, the only confirmed case of animal infection that I know of is a sickened tiger at the Bronx Zoo.
HOW COVID-19 ENDS
- We shouldn’t count on COVID-19 going away naturally when the weather gets warmer. Every recent flu pandemic emerged in the spring or summer months, but secondary waves tended to hit the following winter.
- Even if the COVID-19 virus’s contagiousness drops in the Northern Hemisphere this summer, thanks to warmer, wetter weather, that’s not expected to make a big impact on the pandemic curve.
- Herd immunity would stop the pandemic—when a critical portion of the population is immune to the virus. When there are no longer enough susceptible individuals for a virus to infect, jumping from person to person, the chains of transmission are broken.
- Mass vaccination is the ideal way to accomplish this. Without a vaccine, the only way to achieve herd immunity is through mass infection.
- Based on estimates for the COVID-19 virus from large outbreaks in affected countries and simplistic mathematical models, the minimum population immunity required varies from approximately 30 percent (based on South Korea’s data) to more like 80 percent (based on an estimate from Spain).
- This is why “flattening the curve” is critical. We can’t wait until 80 percent of the population is infected.
- One trait the COVID-19 virus shares with HIV is its rapid mutation rate. The possibility that the virus could transform in the near future to become even more transmissible or dangerous cannot be ruled out.
- A “best guess” estimate presented to the American Hospital Association was about a half a million U.S. deaths if the virus stayed the course. That may be reduced to under 100,000 with sufficient social distancing.
- The CDC developed a Pandemic Severity Index, modelled after the Hurricane Severity Index to define the destructive capacity of a storm. In the 1918 pandemic, about one in three became infected and, of those, about 2 percent died, classifying it as a category 5 pandemic, analogous to a “super typhoon” with sustained winds exceeding 150 miles per hour. COVID-19 infection fatalities are much lower, probably closer to 0.5 percent, meaning 1 in 200 cases dying.
- For more than a century, we’ve known about the pandemic potential of the flu virus, but that 2 percent fatality of the 1918 influenza appears to be the deadliest it ever got. In 1997, however, a flu virus was found in chickens that appears to have killed more than 50 percent of the people it infected. What if a virus like that triggered an outbreak?
PREVENTING FUTURE PANDEMICS: Having Our Meat and Eating It Too
- We were spared by the last pandemic: In 2009, swine flu only triggered a category 1 pandemic, killing a half million people. It did, however, reveal that industrial pork production was a new origin point for pandemic viruses.
- The emergence of H5N1 and other bird flu viruses infecting humans has been blamed on industrial poultry production.
- The CDC considers H7N9, a bird flu virus, to be our gravest pandemic flu threat, one that could kill millions of Americans. To date, H7N9 has killed about 40 percent of the people it has infected. Two in five.
- At this time, neither H5N1 nor H7N9 has acquired the capacity for easy human-to-human transmission, but neither has been eradicated. They’re still out there, still mutating.
- How can we stop the emergence of pandemic viruses in the first place? Whenever possible, treat the cause.
- The largest and oldest association of public health professionals in the world, the American Public Health Association, has called for a moratorium on factory farming for nearly two decades. Its journal published an editorial entitled “The Chickens Come Home to Roost” that went beyond calling for a deintensification of the pork and poultry industries:
“It is curious, therefore, given the pandemic threat, that changing the way humans treat animals, most basically ceasing to eat them, or at the very least, radically limiting the quantity of them that are eaten—is largely off the radar as a significant preventive measure. Such a change, if sufficiently adopted or imposed, could still reduce the chances of the much-feared influenza epidemic. It would be even more likely to prevent unknown future diseases that, in the absence of this change, may result from farming animals intensively and killing them for food. Yet humanity doesn’t even consider this option.”
- This may be changing, thanks to food innovations like plant-based milks, egg products, and meats.
- Our food choices don’t just affect our personal health but our global health. Not just in terms of climate change, but in terms of pandemic risk.
- Major meat producers have started blending in vegetable proteins to make hybrid meats like Tyson’s “Whole Blends” sausage links and Perdue’s “next generation” chicken nuggets. The world’s largest pork producer, Smithfield, recently launched a whole line of plant-based products. Egg-free mayo has taken the sandwich spread sector by storm, and Quorn, a brand of meat-free meat made from the mushroom kingdom, opened a facility capable of producing the meat equivalent of twenty million chickens per year.
- While these products may not be the healthiest from a personal standpoint, they tend to be healthier than their animal-product counterparts and, from a pandemic standpoint, they present zero risk.
- What about cultivated meat? The primary human health benefit of a slaughter-free harvest would be food safety. (If you make meat without intestines, you don’t have to worry about fecal bugs like Salmonella, and if you make meat without lungs, you don’t have to worry about brewing respiratory viruses.) Growing meat directly from muscle cells has been touted for the environmental benefits—reducing water use and greenhouse gas emissions by as much as 96 percent and lower land use by as much as 99 percent—but factoring in pandemic risk, the benefits to human health may rival those to planetary health.
FINAL THOUGHTS
- In the webinar, I ended by taking a moment to acknowledge all of the first responders and frontline medical workers. Many of them are not only dealing with physical and mental exhaustion, the torment of difficult triage decisions, and the pain of losing patients and colleagues, but are also—quite literally—putting their own lives at risk. Thousands of healthcare workers have been infected, and more than a hundred have died.
- Crises like these can bring out the worst in people, like all the hate crimes and harassment against Asian-Americans, but they can also bring out the best.
- You can support those on the front lines from being overwhelmed by staying safe, and, if you can, staying home.
COMING UP NEXT
- During the webinar, I was excited to announce that my entire four-hour lecture will be turned into a month-long series of videos on NutritionFacts.org, so stay tuned.
- I have also been feverishly working on a new book set to be released on May 26, 2020—How to Survive a Pandemic.
- Have any questions? I’ll be going live on Thursday, April 16, at 12pm EDT on Facebook and 6pm EDT on YouTube for special COVID-19 live Q&As.
- I’m working on a second webinar for May. Be sure you’re subscribed to our newsletter to get all of the latest updates first. Click here to subscribe.
(click to enlarge)







This Post Has 4 Comments
https://www.philadelphia.edu.jo/library/directors-message-library
Great selection of modern and classic books waiting to be discovered. All free and available in most ereader formats. download free books
I have read so many posts about the blogger lovers however this post is really a good piece of writing, keep it up
whoah this blog is wonderful i really like reading your articles. Keep up the great paintings! You realize, a lot of people are hunting round for this info, you could help them greatly.